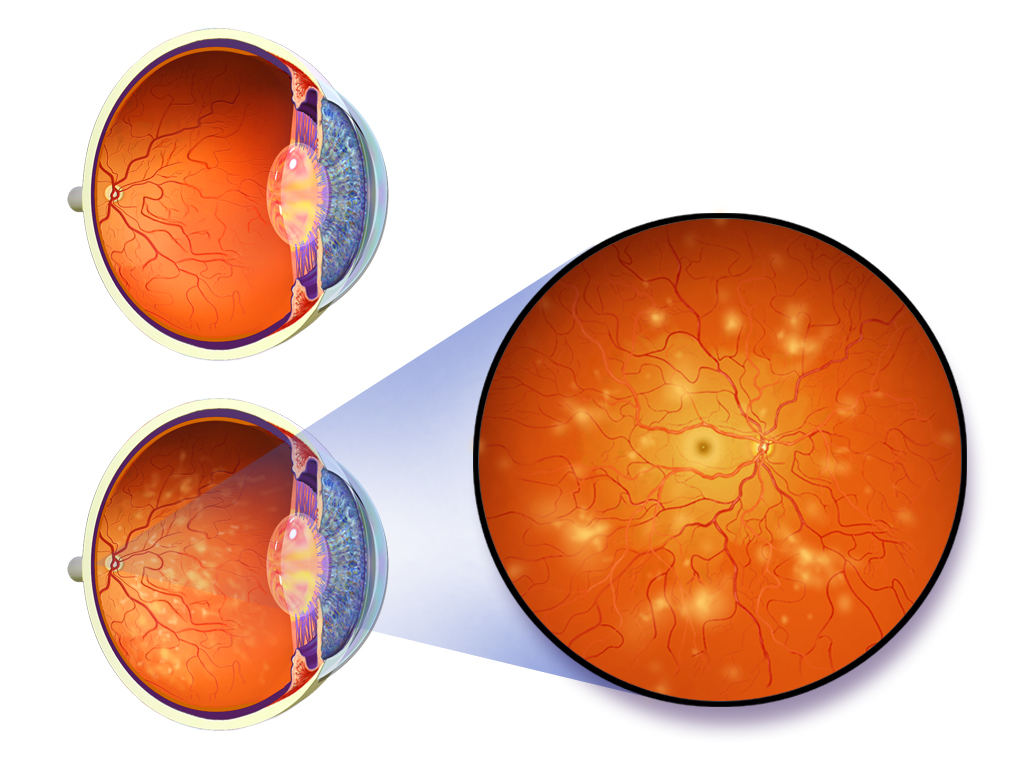
Diabetic Retinopathy
If you have diabetes, you are at risk of developing a preventable eye disease called diabetic retinopathy. Both Type 1 and Type 2 diabetics are at risk of developing diabetic retinopathy, which causes damage to the retina. It is one of the leading causes of vision loss and preventable blindness in adults. Retinopathy is directly correlated with nephropathy (kidney damage) in diabetics, so regular monitoring is of paramount importance.
Diabetic Eye Exams
Diabetic eye exams are a critical part of your eye health care because diabetic eye disease can lead to permanent vision loss if not monitored regularly. Regular annual exams are important in order to catch early signs of retinal damage before it leads to permanent damage. Guidelines state that:
Type 1 patients should be seen within 5 years of diagnosis, and annually thereafter.
Type 2 diabetics should be seen at the time of diagnosis and annually thereafter.
Diabetic Eye Disease Treatment
The best defense against diabetic eye disease is prevention. Ensure you are following your doctor’s recommendations to manage your diabetes, including regulating your blood sugar levels. Good cardiovascular health and blood pressure control will also help reduce the severity of retinopathy. Statistically 60% of diabetics will have some degree of retinopathy 10 years after initial diagnosis.
Mild retinopathy simply requires monitoring and retinal imaging. If your eye exam indicates a need for specialized care then you will be referred to a retina specialist. Depending on the type of retinopathy, you may receive an injection into the back of the eye, or laser treatment to the retina.
Does Alberta health care cover eye exams for diabetes?
Examinations and retinal imaging required explicitly for the management of diabetic eye disease are covered by Alberta Health. However routine comprehensive examinations that include prescriptions for eyewear are NOT funded by the government, regardless of diabetic status. Please call us if you have questions about insurance or Alberta Health coverage.
Diabetes Frequently Asked Questions:
For mild and moderate cases of retinopathy, if blood sugar is lowered and kept stable, signs of retinopathy can improve. For severe non-proliferative and proliferative diabetes, intervention is required to ensure no further damage occurs. This may require referral to a retinal specialist for injections or laser treatment.
Some patients, especially those with type II diabetes, have signs of retinopathy at the time of their diagnosis. Others may take years to develop retinopathy. In many cases, patients begin to show signs of retinopathy after 10 years, even with good blood sugar control.
Usually, patients with diabetes will notice fluctuating vision as the initial symptom of uncontrolled blood sugar. With continued insulin resistance, small vessels in the retina start to become damaged. We use high resolution imaging technologies such as OCT and retinal autofluoresence to look for early signs of damage.
Blurry vision due to high blood sugar will generally improve by lowering and stabilizing your blood sugar levels. However, if retinopathy or fluid leakage within the retina occurs, this may permanently affect your vision. We use OCT technology to take high resolution cross sectional images of your retina to monitor for signs of swelling (retinal edema). If retinal edema is present, you will be referred to a retina specialist for an injection into the eye to reduce the fluid leakage.

